Abstract
Background: Oral mucositis (OM), secondary to mucosal barrier injury of pre-hematopoietic stem cell transplantation (HSCT) conditioning, is a common and painful toxicity of transplantation. Mucositis has been associated with increased risk for infections, hospitalization, analgesia and total parenteral nutrition use, and higher costs. However, prevalence and incidence data for mucositis are inconsistent and underreported. We set to prospectively identify risk factors for oral mucositis in patients undergoing allogeneic HSCT.
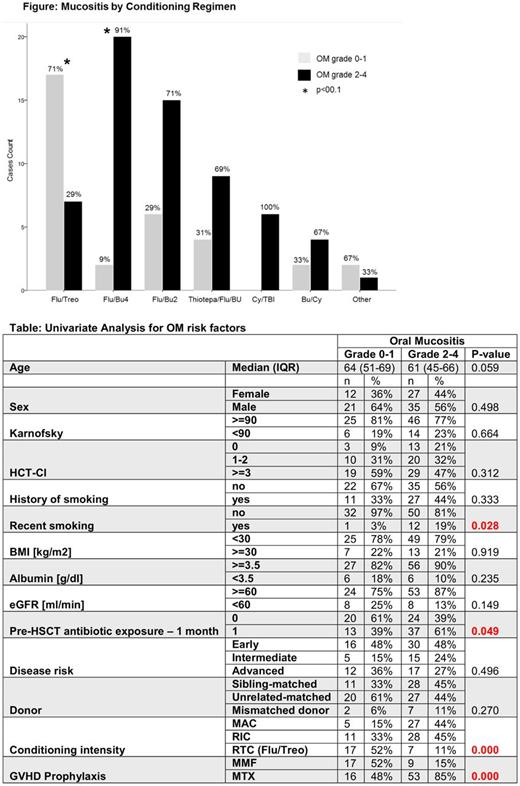
Methods: OM was prospectively evaluated on a weekly basis in patients undergoing allogeneic HSCT. The grade of OM was determined based on the National Cancer Institute Common Toxicity Criteria for Adverse Events (CTCAE) scale (v. 4.0). Severe OM was defined as grade 2 or higher. Conditioning regimens were evaluated individually and according to intensity; myeloablative (MAC), reduced intensity (RIC) or reduced toxicity (RTC). The latter category included only patients receiving Fludarabine and Treosulfan (Flu/Treo). Variables associated with severe OM (p<0.05) were initially identified by univariate analysis (Chi-square and Mann Whitney U tests) and then analyzed in a multivariate logistic regression model. Cox and Fine and Gray regression models were used to study the association between severe OM and overall survival or nonrelapse mortality, respectively.
Results: A total of 95 patients who underwent an allogeneic HSCT from 2016 to 2017 were included. Median age was 61 (range 19-75). Leading indications for HSCT were acute myeloid leukemia (51%), followed by myelodysplastic syndrome (15%), and non-Hodgkin lymphoma (12%). The majority of patients had a comorbidity score ≥3 (51%), were exposed to systemic antibiotics preceding transplantation (53%), and had no history of recent smoking (86.%). Donors were primarily HLA matched unrelated (51.1%) or HLA matched siblings (40%). RIC, MAC, and RTC regimens were used in 41%, 34%, and 25% of the patients, respectively. Methotrexate (MTX) (72.6%) or Mycophenolate mofetil (MMF) (27.4%), in conjunction with Cyclosporine, were given for graft versus host disease (GVHD) prophylaxis. Median follow-up was 165 days (95% CI 130-200).
Median OM grade was 2 (range 0-4), with 65% of the patients experiencing severe mucositis. Median time from HSCT to OM and duration of OM were 8 days (1-14) and 10 days (2-40), respectively. Patients receiving Flu/Busulfan (Bu)-4 days (Flu/Bu4) were more likely to develop severe OM (91% vs. 9%, p<0.01), while among those conditioned with Flu/Treo, 29% had severe OM vs. 71% who did not (p<0.01) (Figure). In a univariate analysis, considering a broad range of patient, disease, and transplant characteristics (Table), only a history of recent smoking (19% vs. 3%, p=0.028), exposure to antibiotics in the preceding month pre-HSCT (61% vs. 39%, p=0.049), and use of MTX for GVHD prophylaxis (85% vs. 49., p<0.001) were associated with severe mucositis. Patients receiving RTC (i.e. Flu/Treo conditioning) had lower rates of severe OM compared to both RIC and MAC (p<0.001). Pre-HSCT albumin levels, obesity, and a low estimated glomerular filtration rate (eGFR) were not associated with OM. In a multivariate logistic regression model use of MTX vs. MMF had an increased risk for severe OM (odds ratio [OR] 11.6 [95% CI 3.2-42.4], p<0.001); compared to MAC, the risk for severe OM was reduced with RTC (OR 0.1 [0.0-0.4], p=0.001. OR for recent smoking was 6.8 (0.7-64.5), with a trend toward statistical significance (p=0.09). Severe OM was not associated with a decrease in short term overall survival (HR 0.59 [95% CI 0.2-1.5] or increase in non-relapse morality (HR 0.51 [0.1-2]).
Conclusion: Our findings suggest that administration of Fludarabine and Treosulfan is an appealing option for conditioning since the risk for oral toxicity is low while intensity is high. Though having a borderline statistical significance, peri-transplantation smoking emerges as an important risk factor for oral mucositis. Therefore, patient counseling about smoking could potentially lower rates of mucositis. In contrast to previous reports, obesity and pre-HSCT albumin and reduced eGFR were not associated with mucositis in our cohort.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal